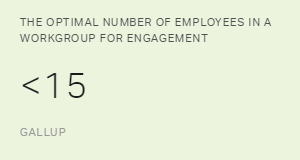
Gallup studies on healthcare organizations indicate that as spans of control
exceed 15 employees, employee engagement levels steadily drop. And, compared
with smaller workgroups, larger workgroups have greater difficulty improving
and maintaining engagement.
On the other hand, Gallup finds that hospitals with engaged staff have
better patient and employee outcomes, including fewer infections, fewer
slips and falls, less turnover, and higher productivity.
So if growing spans of control continue to go unchecked, nurse
and patient outcomes will take a hit. And healthcare leaders will face more
nurse burnout, decreased engagement and increased safety incidents.
Reducing Spans of Control With Clinical Coordinators
One powerful and cost-effective strategy for reducing spans of control
among nurses is implementing a "clinical coordinator" program.
Clinical coordinators are front-line nurses who facilitate ongoing individualized
development -- including goal setting, accountability and strengths coaching
-- with a small group of front-line nurses.
Employees need frequent one-on-one interactions with their managers to
clarify expectations, celebrate successes, identify barriers, maintain
accountability and get immediate feedback.
In fact, Gallup analytics show that employees who strongly agree they have
had conversations with their manager in the past six months about their
goals and successes are 2.8 times more likely to be engaged.
Clinical coordinators are highly accessible, so they can help nurses resolve
challenges and perform their best every day. By asking questions such
as "Is there anything you're struggling with today?" or
"How can I help remove barriers?" and following up on employee
goals, clinical coordinators act as performance coaches who develop, support
and communicate that they care for each caregiver.
For example, clinical coordinators can develop one-on-one connections with
nurses and find learning and development opportunities that match each
nurse's unique aspirations. And, because clinical coordinators maintain
their front-line responsibilities, their peers tend to consider them relatable,
credible and knowledgeable.
Assigning a few hours of weekly managerial work to clinical coordinators
can help healthcare leaders meet employee needs without hiring additional
mid-level managers.
As with every role, to optimize clinical coordinator programs, healthcare
leaders need to
select clinical coordinators who have the right talents and
provide ongoing education and resources to build their capabilities.
Client Story: Cultivating Performance and Modeling Desired Behaviors Using
Clinical Coordinators

Historically, our client Kootenai Health maintained large spans of control
with its nurses. This, however, created barriers to individualized performance
development.
So to proactively invest in each nurse's ongoing development and performance,
based on Gallup's recommendation to reduce spans of control, Kootenai's
leaders gave charge nurses some limited management responsibilities --
and developed the new job description of "clinical coordinator."
To position their clinical coordinators to thrive, Kootenai leaders provide
initial classroom training and ongoing learning and development opportunities.
Leaders also clarify role expectations for clinical coordinators and ensure
their needs are met too.
Under the supervision of nurse managers, each clinical coordinator coaches
and mentors no more than 15 employees.
In addition to their usual responsibilities, clinical coordinators meet
with their nurses for quarterly check-ins to review goals and clarify
expectations. Coaching and mentoring regarding safety concerns occurs
in the moment as much as possible.
Kootenai's clinical coordinators not only support employee development,
they also boost performance as front-line leaders who foster collaboration,
implement changes, model desired behaviors and advance quality initiatives.
Nurses appreciate having
someone to go to -- a trusted adviser who immediately resolves conflicts and answers their
questions quickly.
Since implementing the program in 2015, Kootenai Health has seen meaningful
improvement (0.20 points or greater) in nurse engagement scores.
Seeing how their efforts inspire performance and advance patient outcomes,
many clinical coordinators have discovered an inner passion for leading
and developing others, according to Kootenai Health RN Directors.
As a result, Kootenai leaders expect to see positive effects on succession-planning
efforts and deeper employee alignment with the health system's mission
and purpose.
Gallup can help your organization improve employee engagement and business
outcomes too.